Safely establishing entry into the peritoneal cavity is integral to successful laparoscopic surgery. However, peritoneal access is associated with morbidity, with up to 50% of all surgical complications related to this aspect of laparoscopic surgery (1. Chapron et al 1997; 2, Harkki-Siren et al 1999). The technique that is selected and performed is one for which the surgeon is properly trained and is implemented considering the patient’s body habitus, the type of intraperitoneal pathology, and the risk for adhesions that may involve bowel. Such adhesions are generally related to previous abdominal (laparoscopic or laparotomic) surgical procedures.
WHAT CAN GO WRONG?
Laparoscopic access can often be quite easy, but it is also easy to forget that there exist a plethora of potential complications, particularly those involving bowel and blood vessels. We demonstrate here three adverse outcomes, one a vascular injury secondary to an insufflation needle resulting in a hematoma, one a small bowel injury with a primary access device, and the third an injury to the ileum from insertion of an ancillary port - something that is entirely preventable. These examples should provide adequate incentive to become more than familiar with the instrumentation and appropriate techniques for safe laparoscopic access.
This video shows how trocar-cannula systems can cause bowel injury, even if there is a "so called" safety mechanism. Sticking to surgical principles is paramount to reducing risk.
Access-related injury to retroperitoneal vessels may not manifest in intraperitoneal bleeding - but still can result in profound blood loss.
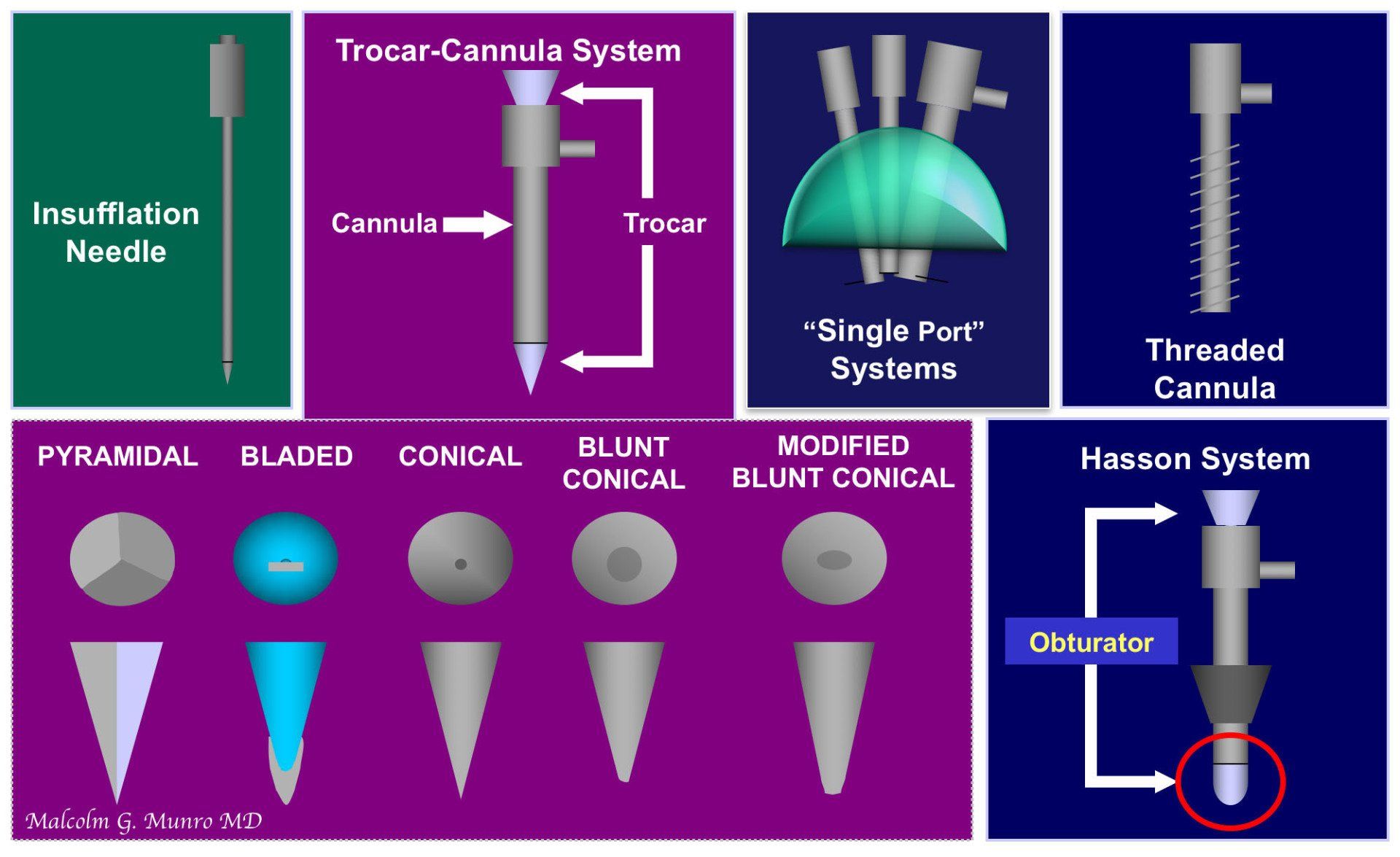
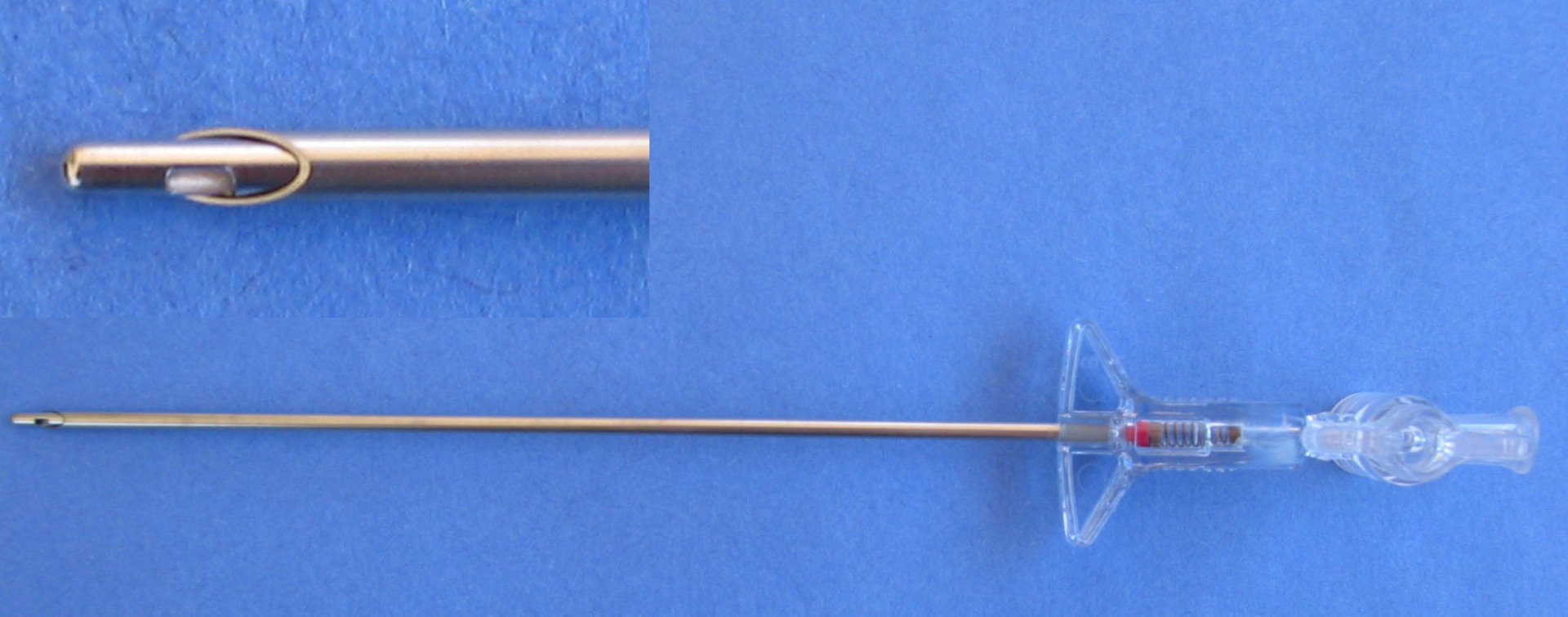
Insufflation Needles
Insufflation needles are devices used to puncture the peritoneum to allow the passage of gas (usually CO2) into the peritoneal cavity. The are necessary for initial portion of the “blind” preinsufflation technique to be discussed subsequently. The original insufflation needle designed by Veress was created to safely empty tuberculous abscesses. The actual Veress needle is a reusable device comprising a hollow needle, about 1.5 mm in outer diameter, an internal obturator with a distal fenestration mounted on a spring allowing it to retract so that the needle can penetrate the abdominal wall. Once the needle is in the peritoneal cavity, tha obturator springs back into position. The other end of the needle has a female Luer component that allows attachment of tubing connected to the CO2 insufflator. For most US institutions, single use insufflation needles are used that are similar to but not identical with the original Veress device.
Primary Access Systems
The laparoscopic cannula (or port) allows laparoscopic instruments to be inserted and removed from the peritoneal cavity without loss of the distending gas. The basic design is a hollow cylindrical structure that contains one or more valves or sealing mechanism at or near its proximal end. For cannulas that are used to transport gas into the peritoneal cavity the design includes a female Luer adapter to allow attachment to the tubing connected with the CO2 insufflator. Large diameter cannulas, particularly those more than 10 mm in inside diameter, are usually designed with adapters or specialized valves to allow the insertion of smaller-diameter instruments without loss of the pneumoperitoneum. The instrument is maintained in the abdominal wall by frictional forces but positional stability can be optimized with a spectrum of outer treatments or designs of the cannula.
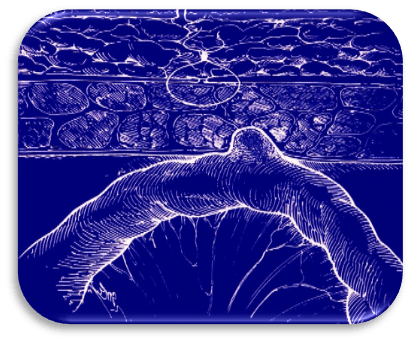
The obturator of the access system is also a cylindrical instrument, but of slightly smaller outside diameter, and longer than the cannula, so that when it is passed fully through the cannula, the tip is exposed. Obturators are called “trocars” when their tip is designed sharp enough to penetrate of the abdominal wall after the creation of a skin incision. Many single use trocar-cannula systems are designed with a pressure-sensitive spring allowing either retraction of the trocar until the peritoneal cavity is reached or deployment of a protective sheath around the tip after peritoneal entry.
None of these “protective” devices has been shown to make insertion safer. The same can be said for clear trocars that allow the laparoscope to be positioned so the entry can be viewed. Unfortunately, these instruments see what has happened, not what will and, as well, have not been shown to provide protection for the patient.
Round tipped blunt obturators are not designed to penetrate the abdominal wall; they are present to facilitate passage of a cannula into the peritoneal cavity when a minilaparotomy technique is used. These devices either have a removable attachment that allows the devices to be temporarily sutured to the abdominal wall, or a balloon device to assist in anchoring the system without sutures. In both instances. A proximally located conical stopper is necessary to seal the incision to prevent escape of the pneumoperitoneum.
Some access cannulas require no obturator, relying on a wood-screw design to penetrate the abdominal wall. These systems substantially reduce, but don’t eliminate the risks of visceral injury.
Ancillary Cannlulas
Ancillary cannulas are necessary to allow the insertion and use of laparoscopic hand instruments such as scissors, probes, and other manipulating devices. Most currently available ancillary cannulas are similar to those designed for insertion of the primary cannula; however, since insufflation may not be necessary many can be made without the Luer insufflation ports, a design that reduces cost, and, for reusable instruments, facilitates the cleaning process.
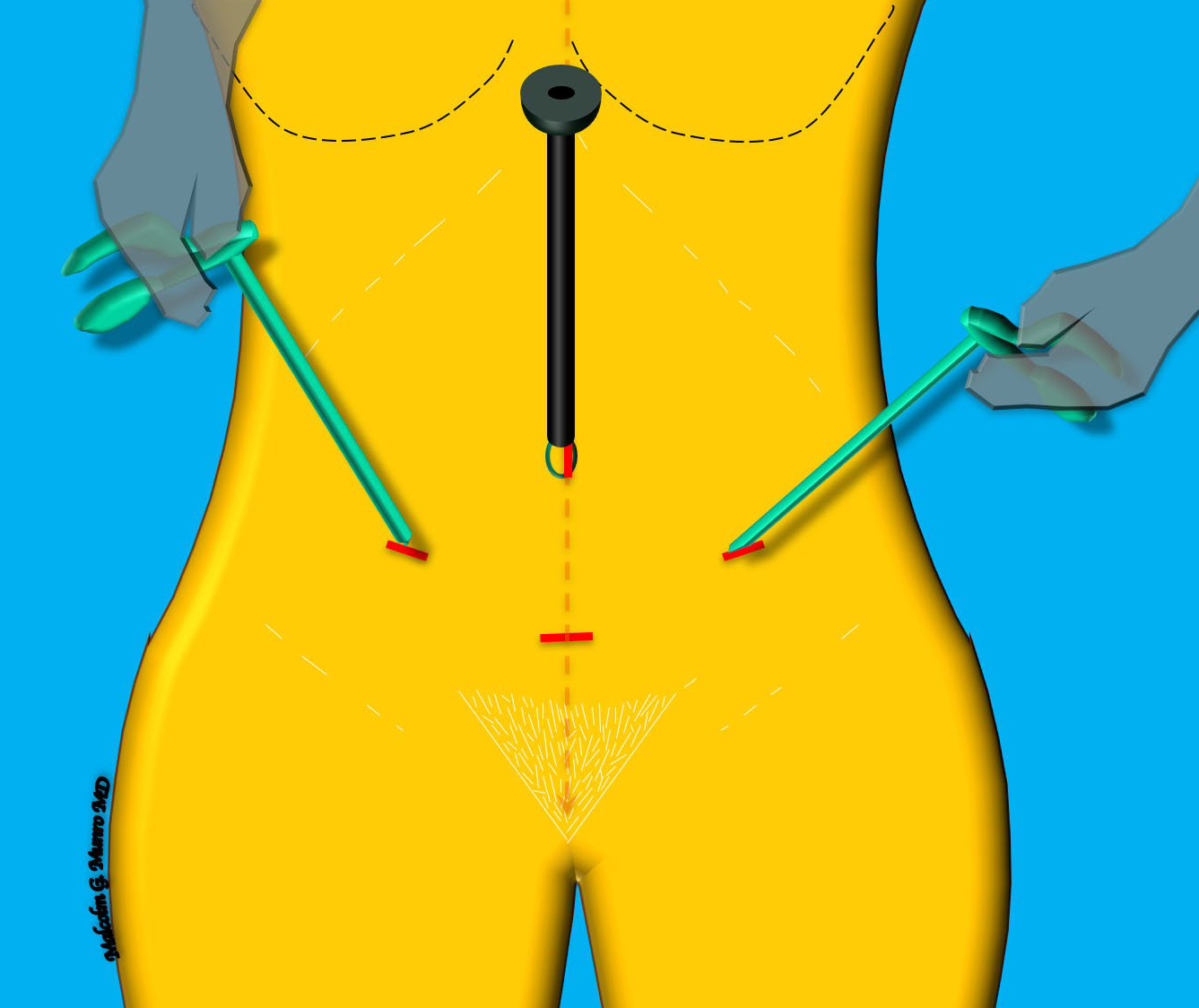
LAPAROSCOPIC ACCESS SITES FOR GYNECOLOGIC SURGERY
For the vast majority of laparoscopic gynecologic surgery, the surgeon selects amongst a set of locations that depend in part upon the pathology to be encountered, the techniques and instruments that will be used and to a degree, the training, experience and "handedness" of the surgeon. It is critically important to understand the vascular and myofascial anatomy of the abdominal wall as well as the course of the great vessels that exist posteriorly in the retroperitoneum. Also important to understand is the impact of body mass index and intraperitoneal pathology on the landmarks which, in turn, may alter technique or location as appropriate to the specific case. Figure 5 demonstrates the typical sites and provides some guidance for landmarks including the umbilicus, the anterior superior iliac spine and other features used to identify the most appropriate access points. Of course, primary access is pivotal, and the one most associated with risk and procedure failure if it isn't accomplished safely and effectively.
PRIMARY ACCESS
Primary peritoneal access for laparoscopic surgery includes establishment of a pneumoperitoneum and placement of the first access port that is used for positioning the laparoscope. There are two main categories of primary access. These are the “open” or minilaparotomy technique named for Harreth Hasson, and a number of blind or “closed” methods that can be categorized as either preinsufflation or “direct entry” techniques. In general, and at least for "blind" techniques, primary access should be performed in the supine position with the long axis of the patient parallel to the floor of the operating room. This means that the Trendelenburg position should NOT be used for primary access. This position displaces the retroperitoneal structures, including the great vessels and can cause the surgeon to direct instruments towards the great vessels near the bifurcation of the aorta.
Blind Technique 1. Preinsufflation
The preinsufflation technique appears to be the most common approach used by gynecologic surgeons (3. Kroft et al 2009). This blind approach starts with insertion of the insufflation needle into the peritoneal cavity through a small incision placed in the skin of the abdominal wall, most commonly in the base of the umbilicus which represents its the thinnest portion.
Before the insufflation needle is passed into the peritoneal cavity the surgeon ensures that the patient is in the supine position, with her back parallel to the floor. The function of the needle’s sprung obturator is checked, the valve opened and a 2-3 mm skin incision is made. The needls is held on the shaft using the the fingers of the dominant hand and at a location that considers the anticipated thickness of the abdominal wall as well as the planned angle of insertion. For umbilical positioning, when the patient has a normal body habitus, the angle of insertion is approximately 45°, increasing to 90° as the BMI increases. Abdominal lift can be provided by the surgeon’s nondominant hand by an assistant although it is not clear that this approach truly reduces the risk of perforation of bowel or blood vessels. The needle is then advanced at the appropriate angle and staying in the sagittal plane, while the surgeon listens for “clicks” created by the obturator when it retracts and releases as it passes through the fascial and peritoneal layers. Should the needle be inserted at a 45° angle through the umbilicus, two such clicks are usually heard.
If the placement is considered satisfactory, the proximal end of the insufflation needle is connected to the CO2 insufflator using hollow tubing and the peritoneal cavity filled to a desired pressure (NOT volume) (3. Kroft et al 2009).
There exists a spectrum of “tests” and signs that purport to confirm that the distal tip of the needle is proper positioned in the peritoneal cavity that include an aspiration test, the hanging drop test, the “hiss” sound test, and the syringe test (4. Fear et al 1968, 5. Lacey 1976, 6. Marret et al 1997). Whereas these tests provide little useful information there exists high quality evidence that an introductory intraperitoneal pressure of less than10 mm Hg is a reliable indicator of correct intraperitoneal placement (7. Ricci et al 1999, 8. Teoh et al 2005). As a result, following activation of the insufflator, the surgical team should ensure that this pressure threshold is confirmed before continuing with the insufflation process.
An elevated initial pressure can occur secondary to omentum occluding the insufflation needle, but surgeons should avoid side to side dislodgement movements in case a perforation has occurred – such a mechanism may result in extension of a 2-mm puncture injury to bowel. When proper positioning of the insufflation needle is unsuccessful, a repeat attempt is reasonable making whatever adjustments – angle or depth of entry – are deemed appropriate. However, the rate of complications including omental, vascular and gastrointestinal injuries, progressively increase with each attempt: 0.8% to 16.3% with one attempt, 16.31% to 37.5% with two attempts, 44.4% to 64% with three attempts and 84.6% to 100% with four attempts(8. Teoh et al 2005). Consequently, gynecologic surgeons should be familiar with a number of methods for achieving primary peritoneal entry switching to an alternative approach after no more than two or three failed entry attempts with the insufflation needle.
The most useful alternative to the umbilicus for primary entry is the left upper quadrant, named Palmer’s point after the French gynecologist who initially described the technique. There are non abdominal sites such as those performed through the vagina including transuterine and trans cul-de-sac methods, but these are rarely used in contemporary surgery. The left upper quadrant is particularly suitable for individuals who have had previous lower abdominal surgery provided (a) there hasn’t been left upper quadrant surgery, and (b) the stomach contents are evacuated with a nasogastric tube. Should surgery have been performed in the left upper quadrant, or in the presence of splenomegaly, the use of ultrasound and the sliding sign (discussed subsequently) may be necessary to identify an appropriate entry point.
Once peritoneal access is successfully established, insufflation is initiated and continued until a predetermined pressure has been reached (9. Thomson et al 2012). It is recommend that this pressure be set at about 20-30 mmHg to allow for safer insertion of ports, but that this pressure be dropped back, preferably to 12 mm Hg before the patient is placed in Trendelenburg’s position (10. Vilos et al 2003, 11. Roy et al 2001, 12. Vilos et al 2017), .
At this point the insufflation needle is removed and the incision lengthened considering the diameter of the selected primary port. The incisional length must be slightly greater than the outside diameter of the port to accommodate its circumference.
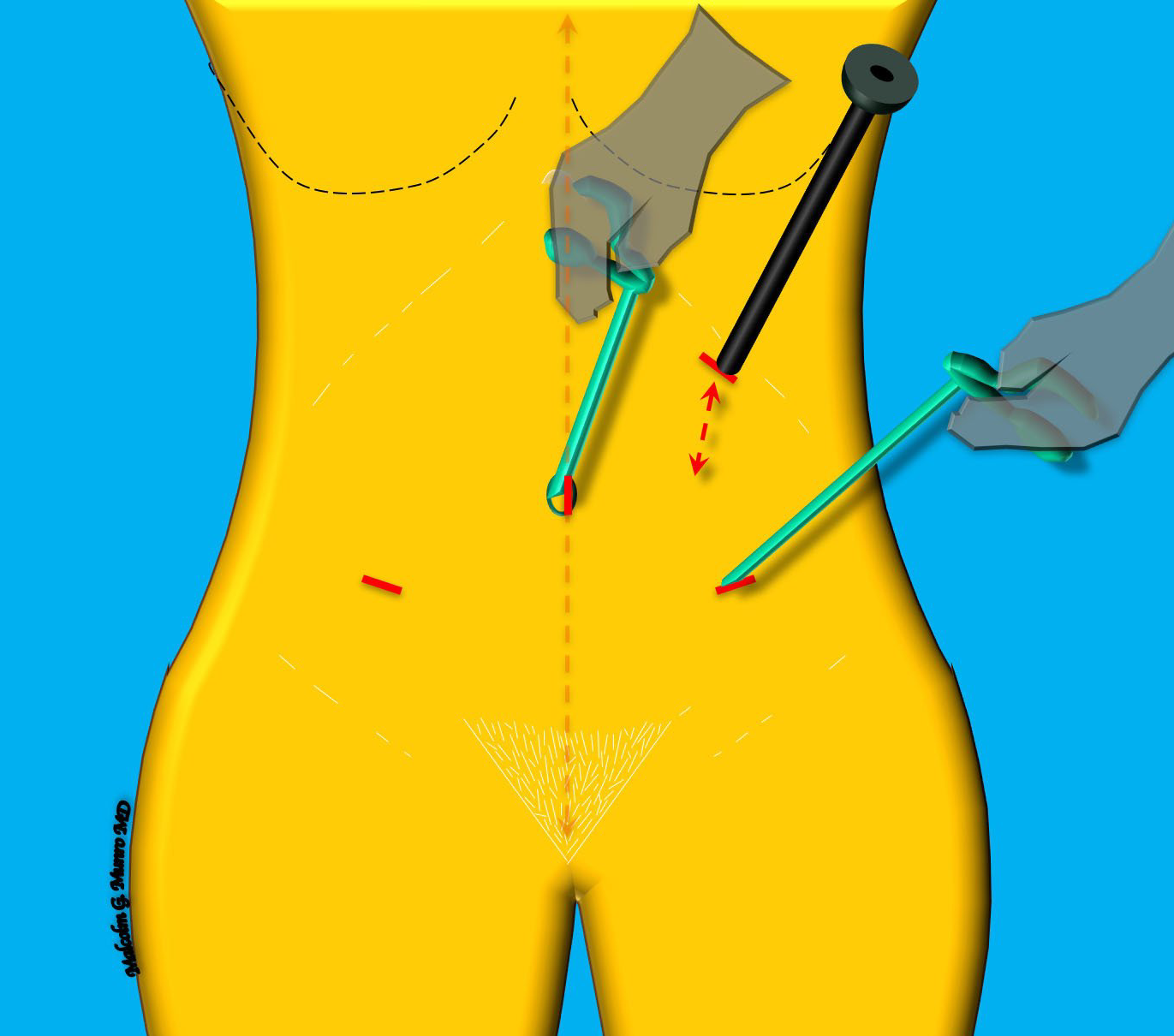
The technique of port insertion varies with the design of the specific system but all must be maintained in a sagittal plane if they are placed through the umbilicus. For most devices, a trocar is placed in and through the port (or cannula) and the assembled system is positioned in the incision and directed towards the peritoneal cavity using the dominant hand at an angle appropriate to the patient’s body habitus. Lifting the abdominal wall is not particularly effective unless the fascia is grasped with tenacious forceps, and unnecessary if the periotoneal cavity is insufflated to 25 – 30 mmHg. The video shows passage of a system with a retractable, single bladed trocar within a 11 mm inside diameter cannula. Note that the thumb and fingers of the non dominant hand are used both to add force and to brake the insertion at a predetermined depth.
It is important to have control of the rate and depth of penetration; the former by avoiding leaning on the device and the latter by braking the insertion either with the index finger of the dominant hand or the fingers of the nondominant hand placed at an appropriate position on the cannula (Figure 6). This "braking" concept should consider the anticipated depth required to access the peritoneal cavity. For smaller hands, and longer trocar-cannula systems, the finger of the dominant hand may not provide adequate depth control. The addition of a second hand can accomplish this task and can also distribute the “work” required allowing the smaller muscles of the forearm to control force – an approach that should improve control while limiting depth. This technique is demonstrated in the accompanying video..
Another way to limit the risk of vascular injury in particular is the use of a trocarless cannula access system (13. Vilos et al 2018). For the trocarless system (EndoTip, Karl Storz Endoscopy, Culver City CA), an appropriate incision is made usually following previous insufflation. The threaded cannula is placed in the incision and the fascia engaged with the horizontally oriented tip. Then the laparoscope can be placed into the empty channel of the cannula. and the device is rotated passing through the remaining layers of the abdominal wall. The abdominal wall can actually be lifted while performing this technique. Entry is confirmed by visualization of the peritoneal cavity. This technique and device will not prevent entry into bowel fused to the abdominal wall, a limitation shared by the minilaparotomy or open technique, but it should essentially eliminate the risk of vascular injury.
The trocarless cannula is one approach, unfortunately not used very much in the US, that essentially eliminates the risk of vascular injury.
Blind Technique 2. Direct Entry
Direct peritoneal entry is a technique that involves positioning the primary port through the abdominal wall and into the peritoneal cavity without prior insufflation. A suitable incision is made, typically in the base of the umbilicus. The specific insertion techniques are similar to those described above for preinsufflation but lifting the abdominal wall is mandatory and should be achieved by grasping and elevating the fascia suitable clamps such as towel clips or Kocher clamps(11. Roy et al 2001). An exception to this is the use of a mini instruments such as the port shown in Figure 3-E that is part of s system that looks similar in function and dimensions to an insufflation needle. This system requires a small caliber laparoscope - 2 mm in outside diameter.
Open or Minilaparotomy Entry (the Hasson method)
The so-called “open laparoscopy” or Hasson technique is based upon the formation of a ‘minilaparotomy’ to achieve primary access (14.
Hasson 1971). The incision is typically about 2 cm in length and placed within or just below the umbilicus and fashioned either transversely or vertically as appropriate. Following creation of the skin incision the surgeon transects the fascia and then the peritoneum with resulting entry into the peritoneal cavity. The procedure is performed with scalpel and scissors all the time under direct visualization. The technique requires a specially designed laparoscopic port (the Hasson Port described above) that can be anchored to the fascia. The system includes a blunt obturator that is used to insert the system and a conical sleeve. Once positioned, the port is secured with sutures placed on either side and secured to the fascia, or, with inflation of an integrated balloon located on the distal tip. These anchoring techniques allow the conical distal sleeve of the cannula to be advanced to seal the fascial incision allowing maintenance of the pneumoperitoneum. When the procedure is completed, the port is removed and the fascial defect closed, usually by tying the same suture.
Another way to reduce the risk of vascular injury is the minilaparotomy or "Hasson" technique. But this is NOT an approach designed to deal with circumstances where there is a high risk of bowel injury (read known or suspected adhesions)
COMPARING PRIMARY ACCESS TECHNIQUES
There is no consensus regarding the most appropriate and safe approach for primary entry into the peritoneal cavity. A Cochrane review last published in 2019, evaluated 57 randomized controlled trials comprising 9,865 subjects (15.
Ahmad et al 2019). While some variations were seen, the evidence failed to show an advantage for any single technique for the prevention of major vascular or visceral complications,. There was also a lower risk of vascular injury (Peto OR 0.13, 95% CI 0.03 to 0.66) and of failed entry (Peto OR 0.21, 95% CI0.14 to 0.30) for minilaparotomy based entry (15.
Ahmad et al 2019). However, the authors noted that the vascular injury analysis varied based on the choice of statistical methodology and as such, any conclusions derived may be unreliable. At the present time, most national organizations, including the Society of Obstetricians and Gynaecologists of Canada (12.
Vilos et al 2017) and the French College of Gynaecologists and Obstetricians (16.
Deffieux et al 2011), suggest that the primary access method should be selected based on surgeon training and preference.
ANCILLARY PORTS
Following establishment of primary access and creation of a pneumoperitoneum is, accessory ports are inserted under direct laparoscopic vision. When positioning lateral ports in the lower quadrants there is a risk of injury to the deep inferior epigastric vessels, a complication that can be largely prevented with attention to the vascular anatomy of the abdominal wall. These vessels can generally be visualized laparoscopically but when the patient is obese, identification may be difficult, and in such cases, the lower quadrant port should be placed based on the anticipated location using other landmarks. These include a distance of ≥ cm from the midline, in McBurney's point (and its mirror image on the left) and lateral to the exit point of the round ligament which lies lateral to the deep epigastric vessels.
Add ancillary ports with temporarily elevated intraperitoneal pressure, under visual direction, and with controlled force.
The anatomical location of the accessory ports is chosen considering a spectrum of factors that include techniques and instruments to be utilized, experience of the assistant and the known or suspected pathology, including the size of an adnexal mass or the uterus. Each of the orientations described below consider the two accessory ports for the primary surgeon and include an umbilical port. However, it should be remembered that the accessory ports can also be a place to position the laparoscope as different ports provide a different view that may be useful during some aspects of a given procedure. In many,, if not most instances a port is positioned ipsilateral to the assistant for traction, irrigation, suction or other maneuvers It is rarely necessary to use anything larger than a 5.5 mm port unless instrumentation dictates otherwise. Curved needles can be passed through 5,5 mm incisions with special techniques, but for efficiency a larger port is often needed. By making the umbilical port the only larger port, the risks of incisional herniation are reduced and there is an lessened cosmetic impact of larger incisions in more visible locations.
Ipsilateral - Midline
The classical positioning of ancillary ports for gynecological laparoscopic surgery comprised an ipsilateral and a suprapubic port with a contralateral port usually used by the assistant. However, such an orientation is ergonomically limiting as the surgeon often experiences fatigue of the shoulder muscles reaching for and manipulating instruments located in the midline, and especially the contralateral port. As a result, some place the midline suprapubic port between the umbilicus and pubic bone, a circumstance that, in Trendelenberg’s position, orients this port closer to the surgeon thereby reducing strain on the upper body.
Ipsilateral - Ipsilateral
Another way to enhance ergonomics is to use ipsilateral-ipsilateral port placement with two ancillary ports on the same side as the primary surgeon. This design reduces muscle fatigue as it allows the surgeon to have both elbows and shoulders in a relaxed position while operating. The upper quadrant port should be placed slightly medial to the ipsilateral lower quadrant port to avoid the inferior epigastric vessels that travel medially after they pass the umbilicus. This orientation allows a larger diameter umbilical port to be used to pass curved needles while visualizing via the left upper quadrant. Furthermore, this port location is compatible with the left upper quadrant entry techniques that are preferred when there exist large masses when previous laparotomies increase the risk of primary umbilical entry by any technique.
Other Considerations
Positioning of ancillary ports can still be associated with adverse events including bladder, bowel and vascular injury. Consequently, and prior to fashioning the incisions, the urinary bladder should be emptied and continuously drained with an indwelling catheter. To minimize the cosmetic impact, the incisions should be fashioned along Langer’s lines; the cleavage lines that indicate the orientation of the underlying dermal collagen fibers. As previously described, the length of the incision should be adequate to allow the formation of a wound circumference adequate circumference compatible for the port being positioned. Confining larger ports to the umbilicus will improve the cosmetic impact and reduce the incidence of hernias, including Richter's hernia where bowel is captured in the peritoneum and preperitoneal fat. All ancillary port insertions should be performed under direct laparoscopic visualization and, while initially, the obturator should be used at a right angle to the fascia to facilitate engagement, the axis of insertion should then be directed toward the surgical field. The risk of “overshooting” and injuring vessels or viscera can be minimized by maintaining the intraperitoneal pressure between 20 and 30 mm. Control using forearm and hand, not shoulder and body weight along with braking techniques should reduce the risks of uncontrolled “over insertion”.
SINGLE PORT TECHNIQUES
The concept of single port laparoscopic surgery is not new and involves the positioning of a single multichannel access system, usually through an umbilical incision. This array includes a port for the laparoscope and two or three for accessory ports through which are passed the hand instruments. So-called “operative laparoscopes” used in the last third of the 20th century comprised an optical channel fibers for illumination as well as an integrated instrument channel, a device that in appearance is much like a contemporary operative hysteroscopic system. This technique is now referred to by several different names, initialisms and acronyms, that include SPA (single port access) and LESS (laparoscopic incision single incision surgery). At this time, the available published comparisons fail to demonstrate any consistent or relevant advantage of surgical procedures performed with single port systems when compared to multiport technique (17. Chung et al 2015) .
The main disadvantages of this approach are related to the alignment of all instruments, a circumstance that limits triangulation, and issues related to the use of RF electrosurgical instruments, particularly those of monopolar design. Instrument makers have redesigned instruments to assist triangulation by making articulated or pre-bent shafts (18. Rao et al 2011). Advances in laparoscopic design can allow articulation of the distal tip by moving the LED light and CMOS sensor elements to the distal end of the device. This eliminates the need for rigid designs based around glass or quartz lenses. (19. Uppal et al 2011).
Activated radiofrequency (RF) monopolar instruments easily create a capacitor involving adjacent devices such as laparoscopes and hand instruments. This circumstance makes vulnerable the bowel lying adjacent to the laparoscope, a circumstance that should exclude the use of monopolar instruments through single port systems.
SPECIAL CIRCUMSTANCES
Previous Abdominal Surgery
Laparoscopic access in a patient with suspected adhesions secondary to prior surgery or peritonitis poses a number of challenges. Evidence exists demonstrating that previous abdominal surgery conveys a high risk of periumbilical adhesions and up to 20% of the time, these include bowel (20. Brill et al 1995, 21. Audebert et al 2000). As a result an alternative access location should be considered with the left upper quadrant being the most appropriate site as long as there is no hepatosplenomegaly and provided the location hasn’t been compromised by previous surgery. Prior to entry, it is necessary to decompress the stomach using a naso- or orogastric tube. In the left upper quadrant the distance between skin and the posterior peritoneum is generally more than 11 cm, but it may be as little as 7 cm in thin individuals and one must consider the location of the left kidney (40). Consequently, the insufflation needle or laparoscopic trocar-cannula system should be inserted in a medially directed fashion, at about a 10-15°angle to avoid the kidney and renal artery. For women of relatively high BMI it can be inserted at a 90° angle to the skin, in thin women, the angle should be reduced to about 45° (22. Giannios et al 2009). The author routinely uses a direct access technique with a 2.5-mm port that has an insufflation needle as the trocar. This can allow confirmation of successful intraperitoneal placement with a 2 mm OD laparoscope. This is the technique recommended by the French College of Gynaecologists and Obstetricians (16. Deffieux et al 2011).
The left upper quadrant point for access is the best way to avoid adhesions - as long as there hasn't been surgery in that area, and provided the stomach is emptied with a nasogastric tube before the insufflation needle or port is positioned.
In some instances, patients with a risk of lower abdominal adhesions will have also had left upper surgery. In such instances extreme care must be taken when contemplating laparoscopic entry. One approach is to use something called the "Visceral Slide Test" whereby the surgeon performs transabdominal ultrasound while the patient takes deep breaths(23. Tu et al 2005, 24. Lee et al 2017, 25. Gerner-Rasmussen et al. 2019) . If the peritoneum and underlying bowel can be seen, an excursion of ≥1 cm is indicative of a location free of adhesions. An extension of this approach is to instill 0.9% Normal saline or preferably Ringer's lactate into the peritoneal cavity via a spinal needle, a circumstance that creates contrast much as is the case with ascites (26. Nezat et al 2009).. Clear spaces can help define the most appropriate insertion location.
Obesity
Obese patients have an umbilicus that is is generally shifted caudal to the underlying aortic bifurcation. If the patient is slightly rotated, the umbilicus can also shift laterally, placing it over to the course of the common iliac vessels (27. Hurd et al 1992). Consequently, when using the blind preinsufflation technique, the surgeon should direct the needle at an angle that is substantially greater than 45°. In very obese individuals this insertion angle should probably reach 90° or perpendicular to the plane of the skin (28. Pasic et al 1999). In such patients and with this technique, it may be even more important to make the incision in the deepest part of the umbilicus as this represents the site possessing the shortest distance between the skin and the peritoneal cavity.
In many obese patients, the abdominal wall thickness in the upper quadrants is less than in the lower quadrants, a circumstance that might make left upper quadrant primary access a safer and more tenable solution.
Thin Patients
The great vessels may lie one to two cm beneath the umbilicus in thin patients, particularly those with a lumbar lordosis (27. Hurd et al 1992). Although peritoneal access is generally considered easier in such patients compared to those who are obese, it is important that the surgeon maintains control over the insufflation needle or trocar-cannula system at the time of entry, limiting the extent of insertion. Such measures should reduce the risk of damage to bowel or major blood vessels. Again, if there are concerns, left upper quadrant or minilaparotomic techniques should be considered.
Pregnancy
With appropriate measures, laparoscopic surgical procedures can be performed safely in pregnant patients, regardless of the trimester. To plan primary peritoneal access, adjust the site of entry must be adjusted in a fashion that accommodates the fundal height of the uterus. With proper adjustment both the preinsufflation and minilaparotomy based techniques can be safely and effectively used (29.
Lemaire et al 1997. 30.
Rollins et al 2004, 31.
Wang et al 2002). However, systems that don’t require an obturator such as the EndoTip® cannula may be particularly suited to these clinical circumstances. Another approach to access in pregnancy is the use of transabdominal ultrasound (32.
Malangoni et al 2003). It is also necessary to adjust the location of ancillary ports to be compatible with the procedure to be performed and to account for the increased size of the uterus.
INCISION MANAGEMENT
The main goals of incision management are to reduce the risk of hernia and dehiscence and to oppose the edges for an optimal cosmetic impact. Additional goals include enhancing healing, minimizing patient discomfort and reducing the need for followup visits. Paragraph
Fascia
There is evidence that hernia and dehiscence can occur with greater frequency with incisions made for laparoscopic ports that have a diameter greater than 10 mm(33. Montz et al 1994). This risk may be reduced by using non-bladed trocar cannula systems(34. Tarnay et al 1999), but, in general, it is recommended that incisions are closed with suture when the port exceeds the 10 mm threshold.There is evidence that hernia and dehiscence can occur with greater frequency with incisions made for laparoscopic ports that have a diameter greater than 10 mm(33. Montz et al 1994). This risk may be reduced by using non-bladed trocar cannula systems(34. Tarnay et al 1999), but, in general, it is recommended that incisions are closed with suture when the port exceeds the 10 mm threshold.
Richter’s hernia occurs when a portion of the bowel is caught in an incision (Figure 9) – a circumstance that can be dangerous because, paradoxically, the symptoms and signs of bowel obstruction don’t occur and acute abdomen may result from a necrotic portion of bowel(35. Murji et al 2017, 36. Regelsberger-Alvarez et al 2020). It is thought that this risk is greater with laparoscopic incisions that are off the midline in the lower or upper quadrants. These observations support the general rule to keep larger incisions in the umbilical region and to close incisions made for ports >10 mm diameter. It may also be appropriate to close incisions made for smaller ports if there have been multiple insertions or removal of large specimens as this may result in enlargement of the defect.
Closure of fascial defects should include the peritoneum as well as the fascia. There are a number of ways to accomplish this, but regardless of the technique, it is important not to incorporate bowel into the closure. Consequently, the abdomen should be elevated and it is useful to keep a laparoscope in one of the small ports, not only to help lift the target area, but to inspect it during or after closure. There are a number of devices that facilitate this process that are too numerous to list here. However, the use of 5/8th curved urological needles and standard needle drivers is an excellent method applicable in most cases.
Skin
There exists a spectrum of techniques for closing skin including absorbable interrupted suture placed transcutaneously or subcuticularly, the appropriate use of tissue adhesive agents and devices such as staples or adhesive strips. In general, staples should be avoided, and adhesive strips alone are not useful deep in the umbilicus. Consequently, small caliber (3-0) absorbable suture placed subcuticuarly or skin adhesives are probably the best choice. Skin adhesives (cyanoacrylate) form a bridge ACROSS the incision, and are NOT applied within the incision. The substance should be applied following careful apposition of tissue and allowed to dry for at least 20 seconds between applications. Three applications are suggested. The accompanying video, while not describing laparoscopic incisional repair, describes the technique accurately.
SUMMARY
Safe access to the peritoneal cavity is essential for successful laparoscopic surgery. Approximately half of all major complications are related to access a circumstance that is generally mitigable with appropriate attention to technique. Implicit in this concept is the ability to recognize at risk patients and appropriately modify the technique used to enter the peritoneal cavity. Also important is to have a predetermined set of steps designed to quickly and effectively deal with visceral or vascular injury should they occur.
REFERENCES
Links to PubMed are found "in-text"
- Chapron CM, Pierre F, Lacroix S, Querleu D, Lansac J, Dubuisson JB. Major vascular injuries during gynecologic laparoscopy. Journal of the American College of Surgeons. 1997;185(5):461-5.
- Harkki-Siren P, Sjoberg J, Kurki T. Major Complications of Laparoscopy: A Follow-Up Finnish Study. Obstetrical & Gynecological Survey. 1999;54(10):632-4.
- Kroft J, Aneja A, Tyrwhitt J, Ternamian A. Laparoscopic peritoneal entry preferences among Canadian gynaecologists. Journal of obstetrics and gynaecology Canada : JOGC = Journal d'obstetrique et gynecologie du Canada : JOGC. 2009;31(7):641-8.
- Fear RECU. Laparoscopy: A Valuable Aid in Gynecologic Diagnosis. Obstetrics & Gynecology. 1968;31(3):297-309.
- Lacey CG. Laparoscopy: a clinical sign for intraperitoneal needle placement. Obstetrics and Gynecology. 1976;47(5):625-7.
- Marret H, Harchaoui Y, Chapron C, Lansac J, Pierre F. Trocar injuries during laparoscopic gynaecological surgery. Report from the French Society of Gynaecological Laparoscopy. Gynaecological Endoscopy. 1998;7(5):235-41.
- Ricci M, Aboolian A. Needle pneumoperitoneum: An alternative technique. Surgical Endoscopy. 1999;13(6):629.
- Teoh B, Sen R, Abbott J. An evaluation of four tests used to ascertain Veres needle placement at closed laparoscopy. Journal of Minimally Invasive Gynecology. 2005;12(2):153-8.
- Thomson AJ, Shoukrey MN, Gemmell I, Abbott JA. Standardizing pneumoperitoneum for laparoscopic entry. Time, volume, or pressure: which is best? J Minim Invasive Gynecol. 2012;19(2):196-200.
- Vilos GA, Vilos AG. Safe laparoscopic entry guided by Veress needle CO2 insufflation pressure. J Am Assoc Gynecol Laparosc. 2003;10(3):415-20.
- Roy GM, Bazzurini L, Solima E, Luciano AA. Safe technique for laparoscopic entry into the abdominal cavity. J Am Assoc Gynecol Laparosc. 2001;8(4):519-28.
- Vilos GA, Ternamian A, Dempster J, Laberge PY. No. 193-Laparoscopic Entry: A Review of Techniques, Technologies, and Complications. J Obstet Gynaecol Can. 2017;39(7):e69-e84.
- Vilos G, Vilos A, Jacob GP, Abu-Rafea B, Ternamian A. Safe Veress Needle Intraperitoneal Placement and Safer Laparoscopic Entry. J Minim Invasive Gynecol. 2018;25(7):1137.
- Hasson HM. A modified instrument and method for laparoscopy. American journal of obstetrics and gynecology. 1971;110(6):886-7.
- Ahmad G, Baker J, Finnerty J, Phillips K, Watson A. Laparoscopic entry techniques. Cochrane Database Syst Rev. 2019;1:CD006583.
- Deffieux X, Ballester M, Collinet P, Fauconnier A, Pierre F, French National College of G, et al. Risks associated with laparoscopic entry: guidelines for clinical practice from the French College of Gynaecologists and Obstetricians. Eur J Obstet Gynecol Reprod Biol. 2011;158(2):159-66.
- Chung JH, Baek JM, Chung K, Park EK, Jeung IC, Chang HT, et al. A comparison of postoperative pain after transumbilical single-port access and conventional three-port total laparoscopic hysterectomy: a randomized controlled trial. Acta Obstet Gynecol Scand. 2015;94(12):1290-6.
- Rao PP, Rao PP, Bhagwat S. Single-incision laparoscopic surgery - current status and controversies. J Minim Access Surg. 2011;7(1):6-16.
- Uppal S, Frumovitz M, Escobar P, Ramirez PT. Laparoendoscopic Single-Site Surgery in Gynecology: Review of Literature and Available Technology. Journal of Minimally Invasive Gynecology. 2011;18(1):12-23.
- Brill AI, Nezhat F, Nezhat CH, Nezhat C. The incidence of adhesions after prior laparotomy: a laparoscopic appraisal. Obstet Gynecol. 1995;85(2):269-72.
- Audebert AJ, Gomel V. Role of microlaparoscopy in the diagnosis of peritoneal and visceral adhesions and in the prevention of bowel injury associated with blind trocar insertion. Fertil Steril. 2000;73(3):631-5.
- Giannios NM, Gulani V, Rohlck K, Flyckt RL, Weil SJ, Hurd WW. Left upper quadrant laparoscopic placement: effects of insertion angle and body mass index on distance to posterior peritoneum by magnetic resonance imaging. Am J Obstet Gynecol. 2009;201(5):522 e1-5.
- Tu FF, Lamvu GM, Hartmann KE, Steege JF. Preoperative ultrasound to predict infraumbilical adhesions: a study of diagnostic accuracy. Am J Obstet Gynecol. 2005;192(1):74-9.
- Lee M, Kim HS, Chung HH, Kim JW, Park NH, Song YS. Prediction of intra-abdominal adhesions using the visceral slide test: A prospective observational study. Eur J Obstet Gynecol Reprod Biol. 2017;213:22-5.
- Gerner-Rasmussen J, Donatsky AM, Bjerrum F. The role of non-invasive imaging techniques in detecting intra-abdominal adhesions: a systematic review. Langenbecks Arch Surg. 2019;404(6):653-61.
- Nezhat C, Cho J, Morozov V, Yeung P, Jr. Preoperative periumbilical ultrasound-guided saline infusion (PUGSI) as a tool in predicting obliterating subumbilical adhesions in laparoscopy. Fertil Steril. 2009;91(6):2714-9.
- Hurd WW, Bude RO, DeLancey JO, Pearl ML. The relationship of the umbilicus to the aortic bifurcation: implications for laparoscopic technique. Obstet Gynecol. 1992;80(1):48-51.
- Pasic R, Levine RL, Wolfe Jr WM. Laparoscopy in morbidly obese patients. Journal of the American Association of Gynecologic Laparoscopists. 1999;6(3):307-12.
- Lemaire BM, van Erp WF. Laparoscopic surgery during pregnancy. Surgical endoscopy. 1997;11(1):15-8.
- Rollins MD, Chan KJ, Price RR. Laparoscopy for appendicitis and cholelithiasis during pregnancy a new standard of care. Surgical Endoscopy. 2004;18(2):237-41.
- Wang CJ, Yen CF, Lee CL, Soong YK. Minilaparoscopic cystectomy and appendectomy in late second trimester. JSLS : Journal of the Society of Laparoendoscopic Surgeons / Society of Laparoendoscopic Surgeons. 2002;6(4):373-5.
- Malangoni MA. Gastrointestinal surgery and pregnancy. Gastroenterology Clinics of North America. 2003;32(1):181-200.
- Montz FJ, Holschneider CH, Munro MG. Incisional hernia following laparoscopy: a survey of the American Association of Gynecologic Laparoscopists. Obstet Gynecol. 1994;84(5):881-4.
- Tarnay CMM, Glass KBM, Munro MGM. Entry Force and Intra-abdominal Pressure Associated With Six Laparoscopic Trocar-Cannula Systems: A Randomized Comparison. Obstetrics & Gynecology. 1999;94(1):83-8.
- Murji A, De Gasperis-Brigante C, Leyland N. Richter's Hernia After Laparoscopic Surgery. J Minim Invasive Gynecol. 2017;24(4):518-9.
- Regelsberger-Alvarez CM, Pfeifer C. Richter Hernia. StatPearls. Treasure Island (FL)2020.